Acute Ischemia Brain
Acute ischemic stroke is a medical emergency that demands immediate attention and treatment. It occurs when there is a sudden blockage in the blood vessels supplying oxygen-rich blood to the brain, leading to a reduction in blood flow and subsequent damage to brain tissue. This condition requires swift intervention to minimize brain injury and preserve neurological function. In this comprehensive guide, we will delve into the intricacies of acute ischemic stroke, exploring its causes, symptoms, diagnosis, treatment options, and long-term management.
Understanding Acute Ischemic Stroke

Acute ischemic stroke is a complex neurological event that arises from various underlying conditions and risk factors. It is characterized by the abrupt interruption of blood flow to a specific region of the brain, typically due to a blockage or occlusion in one of the cerebral arteries. The resulting deprivation of oxygen and nutrients to brain cells can lead to rapid tissue damage and potential permanent disability or death.
The brain is an incredibly energy-intensive organ, requiring a constant supply of oxygen and glucose to function properly. Even a brief interruption in blood flow can lead to irreversible damage, as brain cells are highly sensitive to ischemia (reduced blood supply). The longer the brain is deprived of oxygen, the greater the extent of damage and potential loss of neurological function.
Causes and Risk Factors
Acute ischemic stroke can arise from a range of underlying conditions, with the most common being atherosclerosis, a process where plaque builds up in the arteries, narrowing and hardening them over time. This plaque can eventually rupture, leading to the formation of a blood clot that blocks blood flow to the brain.
Other potential causes include embolisms, where a blood clot or other debris travels through the bloodstream and becomes lodged in a cerebral artery, and dissection, a condition where the layers of an artery tear apart, causing blood to flow between the layers and blocking the vessel. Additionally, certain medical conditions such as atrial fibrillation, heart valve problems, and certain blood disorders can increase the risk of stroke by promoting the formation of blood clots.
Several risk factors contribute to the development of acute ischemic stroke. Age is a significant factor, with the risk increasing as individuals grow older. Additionally, certain lifestyle factors, such as smoking, excessive alcohol consumption, and physical inactivity, can elevate the risk. Uncontrolled high blood pressure, high cholesterol, diabetes, and obesity are also major risk factors, as they contribute to the development of atherosclerosis and other cardiovascular diseases.
Symptoms and Recognition
Recognizing the symptoms of acute ischemic stroke is crucial for timely intervention. The onset of symptoms is typically sudden and may include weakness or paralysis on one side of the body, facial drooping, difficulty speaking or understanding speech, vision problems, severe headache, dizziness, and loss of balance or coordination. These symptoms often occur suddenly and can vary in severity.
It is important to note that the specific symptoms experienced may depend on the location and extent of the stroke. For instance, a stroke affecting the right side of the brain may lead to weakness or paralysis on the left side of the body, while a stroke in the left hemisphere may result in language and speech difficulties. Prompt recognition and response to these symptoms can significantly impact the outcome and potential for recovery.
Diagnosis and Assessment

Diagnosing acute ischemic stroke involves a comprehensive evaluation to determine the presence and extent of the stroke, as well as the underlying cause. The diagnostic process typically begins with a thorough medical history and physical examination to assess neurological function and identify potential risk factors.
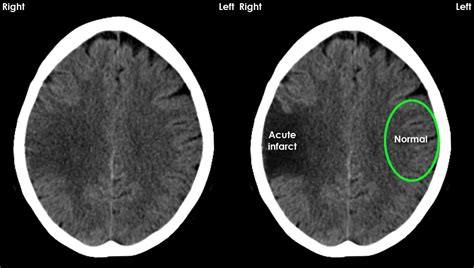
Neuroimaging Techniques
Neuroimaging plays a pivotal role in diagnosing acute ischemic stroke. Computed Tomography (CT) scans are often the first-line imaging modality, providing detailed images of the brain and helping to identify the presence of bleeding or other abnormalities. Magnetic Resonance Imaging (MRI) scans offer even greater sensitivity and can detect small strokes that may be missed by CT scans.
| Imaging Technique | Description |
|---|---|
| CT Scan | Provides detailed images of the brain, useful for identifying bleeding or large strokes. |
| MRI Scan | Offers greater sensitivity, detecting small strokes and providing detailed information on brain tissue damage. |

In addition to these imaging techniques, specialized MRI sequences, such as diffusion-weighted imaging (DWI) and perfusion-weighted imaging (PWI), can provide valuable information about the extent of the stroke and the potential for recovery. DWI can identify areas of acute ischemia, while PWI can assess the blood flow to the brain, helping to guide treatment decisions.
Laboratory Tests and Vascular Imaging
Laboratory tests, such as complete blood counts, coagulation studies, and cardiac enzymes, are often ordered to assess the overall health of the patient and to identify potential underlying causes of the stroke. Additionally, vascular imaging techniques, such as carotid ultrasound and cerebral angiography, can provide detailed information on the blood vessels supplying the brain, helping to identify blockages or abnormalities.
Treatment and Management
The treatment of acute ischemic stroke aims to restore blood flow to the brain, minimize brain damage, and prevent further complications. The type of treatment and its timing depend on various factors, including the severity of the stroke, the time since symptom onset, and the patient’s overall health.
Thrombolytic Therapy
Thrombolytic therapy, also known as clot-busting treatment, is a crucial intervention for acute ischemic stroke. This treatment involves the administration of a medication, such as tissue plasminogen activator (tPA), which dissolves the blood clot and restores blood flow to the affected area of the brain. The effectiveness of thrombolytic therapy is time-dependent, with the best outcomes achieved when treatment is initiated within 4.5 hours of symptom onset.
However, thrombolytic therapy is not without risks. It can lead to bleeding complications, including intracranial hemorrhage, and is therefore carefully selected for patients who are most likely to benefit from the treatment while minimizing potential risks.
Mechanical Thrombectomy
For patients who are not eligible for or do not respond to thrombolytic therapy, mechanical thrombectomy may be an option. This procedure involves the use of specialized devices, such as stent retrievers or aspiration catheters, to physically remove the blood clot and restore blood flow. Mechanical thrombectomy is typically reserved for patients with large vessel occlusions and is often performed in conjunction with thrombolytic therapy.
Stroke Unit Care and Rehabilitation
Following the acute phase of treatment, patients with acute ischemic stroke often require specialized care in a stroke unit or intensive care unit. This care aims to stabilize the patient, manage potential complications, and initiate rehabilitation to optimize recovery. Stroke unit care involves a multidisciplinary team, including neurologists, nurses, physiotherapists, occupational therapists, and speech therapists, who work together to address the patient’s unique needs and challenges.
Rehabilitation is a critical component of stroke management, as it aims to restore lost functions and improve the patient's quality of life. Rehabilitation programs are tailored to the individual's needs and may include physical therapy to improve strength, balance, and coordination, occupational therapy to enhance daily living skills, and speech therapy to address language and communication difficulties.
Prevention and Long-Term Management
Preventing acute ischemic stroke is crucial, as it can significantly reduce the risk of recurrence and improve long-term outcomes. Primary prevention focuses on reducing the risk factors associated with stroke, while secondary prevention aims to prevent recurrence in individuals who have already experienced a stroke.
Lifestyle Modifications
Lifestyle modifications play a vital role in stroke prevention. Smoking cessation is a key intervention, as smoking significantly increases the risk of stroke and other cardiovascular diseases. Adopting a healthy diet, rich in fruits, vegetables, whole grains, and lean proteins, can help control blood pressure, cholesterol, and weight, reducing the risk of atherosclerosis and stroke.
Regular physical activity is also essential, as it helps maintain a healthy weight, improves cardiovascular health, and reduces the risk of diabetes and other metabolic disorders. Additionally, stress management and adequate sleep are important factors in stroke prevention, as they can impact blood pressure and overall cardiovascular health.
Medication and Surgical Interventions
Medication plays a crucial role in stroke prevention, particularly for individuals with underlying cardiovascular conditions. Antiplatelet medications, such as aspirin or clopidogrel, are often prescribed to reduce the risk of blood clot formation. For individuals with atrial fibrillation or other cardiac conditions, anticoagulant medications, such as warfarin or direct oral anticoagulants (DOACs), may be recommended to prevent the formation of blood clots.
In certain cases, surgical interventions may be necessary to prevent stroke. Carotid endarterectomy, for example, is a procedure to remove plaque from the carotid arteries, reducing the risk of stroke in individuals with significant carotid artery stenosis. Additionally, for individuals with certain heart conditions, such as patent foramen ovale (PFO), closure of the defect may be recommended to reduce the risk of stroke.
Conclusion

Acute ischemic stroke is a complex and time-sensitive condition that requires prompt recognition, diagnosis, and treatment. By understanding the causes, symptoms, and treatment options, healthcare professionals can provide the best possible care for patients with acute ischemic stroke. Additionally, by implementing effective prevention strategies and long-term management plans, the risk of recurrence can be significantly reduced, improving the overall quality of life for individuals affected by this condition.
What are the long-term effects of acute ischemic stroke?
+
The long-term effects of acute ischemic stroke can vary widely depending on the severity and location of the stroke. Common long-term effects include physical disabilities such as weakness or paralysis, cognitive impairments like memory loss or difficulty concentrating, and emotional or behavioral changes. Rehabilitation and ongoing medical care can help manage these effects and improve quality of life.
How can I reduce my risk of having an acute ischemic stroke?
+
Reducing your risk of acute ischemic stroke involves adopting a healthy lifestyle and managing any underlying medical conditions. This includes maintaining a healthy weight, engaging in regular physical activity, quitting smoking, managing stress, and controlling conditions such as high blood pressure, high cholesterol, and diabetes. Regular check-ups with your healthcare provider are also important for monitoring and managing risk factors.
What are the potential complications of acute ischemic stroke?
+
Acute ischemic stroke can lead to various complications, including recurrent strokes, infections such as pneumonia, deep vein thrombosis, and urinary tract infections. Additionally, stroke can cause long-term complications such as depression, anxiety, and post-stroke fatigue. Prompt medical attention and proper management can help prevent and manage these complications.
Can acute ischemic stroke be prevented entirely?
+
While acute ischemic stroke cannot be completely prevented, taking proactive measures to address risk factors can significantly reduce the likelihood of experiencing a stroke. This includes adopting a healthy lifestyle, managing underlying medical conditions, and working closely with healthcare professionals to monitor and control risk factors.



