Celiac Disease And Medications
Celiac disease is a complex autoimmune disorder that affects millions of people worldwide. It is a condition where the ingestion of gluten, a protein found in wheat, barley, and rye, triggers an immune response that damages the small intestine. This disease requires strict adherence to a gluten-free diet for lifelong management. However, the impact of celiac disease extends beyond dietary restrictions, and it can also influence the way medications are metabolized and absorbed by the body.
This comprehensive article delves into the intricate relationship between celiac disease and medications, exploring how this autoimmune disorder can affect drug efficacy, interactions, and overall treatment outcomes. By understanding these connections, individuals with celiac disease, healthcare professionals, and the pharmaceutical industry can make informed decisions to ensure optimal health and treatment success.
Understanding Celiac Disease and Its Impact on the Body

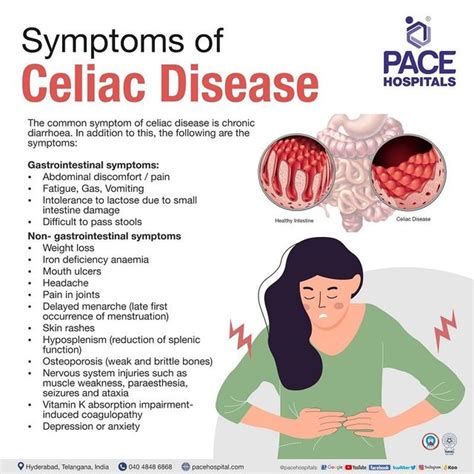
Celiac disease is an often-misunderstood condition, with its symptoms and complications varying widely among individuals. While the primary trigger is gluten, the disease’s impact on the body goes far beyond the gastrointestinal system. The autoimmune response caused by gluten ingestion can lead to a range of symptoms, including diarrhea, abdominal pain, fatigue, and malnutrition.
In individuals with celiac disease, the ingestion of gluten triggers an immune reaction that attacks the small intestine's villi, tiny finger-like projections that line the intestinal wall. This immune response causes inflammation and damage to the villi, leading to a reduction in their surface area. As a result, the intestine's ability to absorb nutrients from food is compromised, leading to malabsorption issues and a range of associated health problems.
The impact of celiac disease is not limited to the gastrointestinal tract. The disease can also affect other organs and systems in the body, including the nervous system, skin, liver, and even the reproductive system. This widespread effect makes managing celiac disease a complex task that requires a holistic approach to healthcare.
One of the most challenging aspects of celiac disease is the potential for long-term complications if the condition is left untreated or managed improperly. Over time, the persistent inflammation and damage to the small intestine can lead to serious health issues, including anemia, osteoporosis, infertility, and an increased risk of certain types of cancer. Therefore, it is crucial for individuals with celiac disease to adhere to a strict gluten-free diet and manage their condition effectively.
The Complex Relationship Between Celiac Disease and Medications

When it comes to medications, individuals with celiac disease face unique challenges. The damage to the small intestine’s villi can affect the absorption and metabolism of drugs, potentially impacting their effectiveness and safety. This complex relationship between celiac disease and medications is an area of growing interest and research in the medical community.
One of the primary concerns is the potential for drug-nutrient interactions. Celiac disease can lead to deficiencies in essential nutrients, such as vitamins and minerals, which are crucial for the body's normal functioning and drug metabolism. For instance, vitamin B12, which is essential for the proper functioning of the nervous system and red blood cell production, is often deficient in individuals with celiac disease. This deficiency can impact the metabolism of certain medications, potentially reducing their effectiveness.
Additionally, the malabsorption issues associated with celiac disease can affect the absorption of orally administered medications. The damaged intestinal lining may not effectively absorb certain drugs, leading to reduced blood levels of the medication and, consequently, decreased therapeutic effect. This can be particularly problematic for medications that require precise dosing, such as those used to manage cardiovascular conditions or psychiatric disorders.
Another aspect to consider is the potential for drug-induced intestinal damage in individuals with celiac disease. Some medications, particularly those with gastrointestinal side effects, can exacerbate the existing intestinal damage caused by celiac disease. This can lead to further inflammation and potentially worsen the symptoms and complications associated with the disease.
Drug Efficacy and Celiac Disease
The impact of celiac disease on drug efficacy is a critical area of study. Research has shown that certain medications may not work as effectively in individuals with celiac disease due to the altered intestinal environment. For instance, studies have suggested that the efficacy of oral contraceptives may be reduced in women with celiac disease due to malabsorption issues.
Furthermore, the damage to the intestinal lining can affect the body's ability to absorb and utilize certain nutrients that are essential for the proper functioning of medications. For example, celiac disease can lead to deficiencies in folic acid, a vitamin crucial for the body's synthesis of DNA and RNA. This deficiency can impact the effectiveness of medications that rely on folic acid for their action, such as certain anti-epileptic drugs.
It is important to note that not all medications are affected equally by celiac disease. The impact of the disease on drug efficacy can vary depending on the specific medication, the route of administration, and the individual's overall health status. Therefore, it is crucial for healthcare professionals to carefully consider these factors when prescribing medications to individuals with celiac disease.
| Medication Category | Potential Impact of Celiac Disease |
|---|---|
| Oral Contraceptives | Reduced efficacy due to malabsorption issues |
| Anti-epileptic Drugs | Potential impact on drug action due to folic acid deficiency |
| Cardiovascular Medications | May require precise dosing due to altered absorption |
| Psychiatric Medications | Potential for reduced therapeutic effect |

Drug Interactions and Celiac Disease
Celiac disease can also influence drug interactions, both with other medications and with certain foods or supplements. The altered intestinal environment in individuals with celiac disease can affect the metabolism and elimination of drugs, potentially leading to unexpected interactions.
For example, certain medications that are metabolized in the liver may have their metabolism affected by celiac disease. This is because the liver plays a crucial role in drug metabolism, and celiac disease can impact liver function due to the associated nutrient deficiencies and inflammation. As a result, the metabolism of these medications may be altered, potentially leading to increased or decreased drug levels in the body.
Additionally, the use of certain medications in individuals with celiac disease may require adjustments to their gluten-free diet. For instance, some medications may contain gluten as an inactive ingredient, which can trigger an immune response in individuals with celiac disease. In such cases, healthcare professionals may need to prescribe alternative medications or advise patients on how to manage their diet while taking these medications.
It is crucial for individuals with celiac disease to inform their healthcare providers about all the medications they are taking, including over-the-counter drugs, supplements, and herbal remedies. This information is essential for healthcare professionals to make informed decisions about drug interactions and to ensure the safe and effective management of the disease.
Managing Medications for Individuals with Celiac Disease
Given the unique challenges posed by celiac disease, managing medications for individuals with this condition requires a tailored approach. Healthcare professionals must carefully consider the potential impact of celiac disease on drug efficacy, interactions, and absorption when prescribing medications.
One of the key strategies is to ensure a comprehensive medication review for individuals with celiac disease. This involves a thorough assessment of the patient's medical history, current medications, and any potential interactions or absorption issues. By conducting a detailed medication review, healthcare professionals can identify any medications that may require adjustments or alternatives to ensure optimal treatment outcomes.
Additionally, healthcare providers should educate individuals with celiac disease about the potential impact of their condition on medications. This includes providing information on drug-nutrient interactions, the importance of adherence to a gluten-free diet, and the need for regular monitoring of medication levels and effectiveness. Empowering patients with this knowledge can help them actively participate in their healthcare decisions and management.
For individuals with celiac disease, it is crucial to maintain open communication with their healthcare team. This includes regularly discussing any changes in their health status, medication side effects, or concerns about drug interactions. By fostering a collaborative relationship with their healthcare providers, individuals with celiac disease can ensure that their medication management is optimized for their unique needs.
Personalized Medication Plans
Due to the variability in celiac disease symptoms and complications, there is no one-size-fits-all approach to medication management. Each individual with celiac disease may require a personalized medication plan that takes into account their specific health needs, the severity of their disease, and any associated conditions or complications.
For instance, individuals with celiac disease who also have osteoporosis may require medications to manage both conditions. In such cases, healthcare professionals must carefully consider the potential interactions between osteoporosis medications and other drugs being taken by the patient. This may involve adjusting dosages, timing of medication administration, or prescribing alternative medications to minimize the risk of adverse events.
Personalized medication plans also take into account the individual's response to medications. Some individuals with celiac disease may require higher doses of certain medications due to malabsorption issues, while others may have a heightened sensitivity to certain drugs. Regular monitoring and adjustments to medication regimens are essential to ensure the best possible outcomes for each patient.
The Role of Nutritional Support
Nutritional support plays a critical role in managing celiac disease and its impact on medications. Ensuring adequate nutrient intake can help mitigate the potential drug-nutrient interactions and malabsorption issues associated with the disease.
For example, individuals with celiac disease may benefit from supplements to address specific nutrient deficiencies. This could include vitamin B12, iron, calcium, or vitamin D supplements, depending on the individual's needs. By addressing these deficiencies, the body's ability to metabolize and utilize medications can be optimized, potentially improving the efficacy of the drugs.
Furthermore, a well-balanced gluten-free diet can help support overall health and improve the functioning of the intestinal lining. This, in turn, can enhance the absorption of orally administered medications, ensuring that they reach their intended therapeutic levels in the body. Healthcare professionals should work closely with patients to develop a nutritional plan that meets their specific needs and supports their overall health and medication management.
The Future of Celiac Disease and Medication Management
As our understanding of celiac disease and its impact on medications continues to evolve, so too do the strategies for managing this complex condition. The future of celiac disease management holds promise for improved patient outcomes and a more holistic approach to healthcare.
Precision Medicine and Celiac Disease
The concept of precision medicine, which tailors medical treatment to individual characteristics, holds great potential for managing celiac disease. By considering an individual’s genetic makeup, lifestyle factors, and specific disease characteristics, healthcare professionals can develop personalized treatment plans that maximize the effectiveness of medications while minimizing potential risks.
For instance, genetic testing can identify specific genetic variations that may influence an individual's response to certain medications. This information can be used to guide medication choices and dosages, ensuring that the selected drugs are well-tolerated and effective for the individual. Precision medicine approaches can also help identify potential drug-gene interactions, further refining the medication management plan for individuals with celiac disease.
Advancements in Drug Delivery Systems
Advancements in drug delivery systems offer new opportunities for managing celiac disease and its impact on medications. For example, the development of targeted drug delivery systems can enhance the absorption and efficacy of medications, even in individuals with compromised intestinal function due to celiac disease.
One promising approach is the use of nanoparticle-based drug delivery systems. These nanoparticles can be engineered to deliver medications directly to the site of action, bypassing the damaged intestinal lining and ensuring optimal drug absorption. This technology has the potential to revolutionize medication management for individuals with celiac disease, improving drug efficacy and reducing the risk of adverse effects.
Patient Education and Empowerment
Empowering individuals with celiac disease through education is a cornerstone of future management strategies. By providing patients with comprehensive information about their condition, medications, and potential interactions, healthcare professionals can foster a sense of control and engagement in their healthcare journey.
Educational initiatives can include workshops, online resources, and support groups specifically designed for individuals with celiac disease. These resources can cover a range of topics, from understanding the disease and its complications to managing medications effectively. By empowering patients with knowledge, they can actively participate in their treatment decisions and take a proactive approach to managing their health.
Conclusion: A Holistic Approach to Celiac Disease Management

Celiac disease is a complex condition that requires a comprehensive and holistic approach to management. From dietary adjustments to medication management and nutritional support, every aspect of an individual’s healthcare needs to be carefully considered and tailored to their unique circumstances.
The relationship between celiac disease and medications is an area of ongoing research and innovation. By understanding the potential impact of celiac disease on drug efficacy, interactions, and absorption, healthcare professionals can make informed decisions to optimize treatment outcomes for individuals with this condition.
As we continue to advance our understanding of celiac disease and develop new strategies for management, the focus remains on improving patient outcomes and quality of life. With a combination of personalized medication plans, precision medicine approaches, and patient empowerment, the future of celiac disease management looks promising, offering hope and improved health for those living with this condition.
How does celiac disease affect the absorption of medications?
+Celiac disease can impact the absorption of medications due to the damage it causes to the small intestine’s villi. This damage can lead to reduced surface area for absorption, potentially affecting the efficacy of orally administered drugs.
What are the potential drug-nutrient interactions in individuals with celiac disease?
+Celiac disease can lead to nutrient deficiencies, such as vitamin B12 and folic acid, which are essential for the proper functioning of certain medications. These deficiencies can impact the metabolism and effectiveness of these drugs.
How can healthcare professionals manage medications for individuals with celiac disease?
+Healthcare professionals should conduct comprehensive medication reviews, educate patients about potential interactions, and develop personalized medication plans that consider the individual’s specific health needs and the impact of celiac disease on medication efficacy.



