Cranial Fluid Pressure

Understanding cranial fluid pressure is crucial for anyone interested in neuroscience, medicine, or even just general health. It's a topic that often raises questions and concerns, as it plays a vital role in our overall well-being. This article aims to provide an in-depth exploration of cranial fluid pressure, covering its mechanisms, potential issues, and the latest research and advancements in the field.
The Basics of Cranial Fluid Pressure
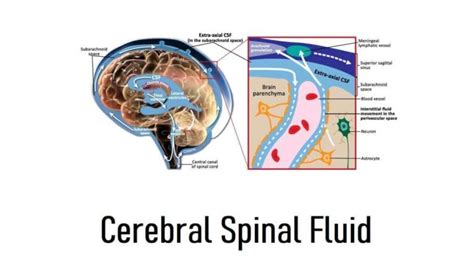
Cranial fluid pressure, also known as intracranial pressure (ICP), refers to the force exerted by the cerebrospinal fluid (CSF) within the skull. CSF is a clear, colorless fluid that surrounds the brain and spinal cord, providing cushioning and nourishment. It’s produced in the brain’s ventricles and circulates through a network of channels and spaces, eventually being absorbed back into the bloodstream.
The balance of CSF production and absorption is crucial for maintaining normal intracranial pressure. When this balance is disrupted, it can lead to a range of issues, from mild headaches to severe neurological conditions.
Regulation of Cranial Fluid Pressure
The body has intricate mechanisms to regulate ICP. One of the primary regulators is the choroid plexus, a network of capillaries located in the brain’s ventricles. The choroid plexus produces CSF at a rate that, under normal circumstances, matches the absorption rate, thus maintaining a stable pressure within the cranial cavity.
Additionally, the brain's ability to adjust its volume in response to changes in CSF pressure is crucial. This process, known as cerebral autoregulation, ensures that blood flow to the brain remains constant despite fluctuations in blood pressure and ICP. It's a complex mechanism involving various vascular and neural factors.
| CSF Production Rate (μL/min) | Absorption Rate (μL/min) |
|---|---|
| 20-30 | 20-30 |

Causes of Increased Cranial Fluid Pressure

Abnormal increases in intracranial pressure can result from various conditions and factors. One common cause is hydrocephalus, a condition characterized by the abnormal accumulation of CSF within the brain’s ventricles. This can be due to an overproduction of CSF or a blockage in its normal flow, leading to an increase in pressure and potential brain damage.
Traumatic brain injuries (TBIs) are another major cause of elevated ICP. When the brain sustains a significant impact, it can lead to swelling and inflammation, which, in turn, increases pressure within the confined space of the skull. If left untreated, this can have severe consequences, including brain damage and even death.
Other Factors and Conditions
- Brain tumors: The growth of a tumor within the skull can occupy space and compress surrounding tissues, leading to increased ICP.
- Brain infections: Inflammation caused by infections such as meningitis or encephalitis can result in increased pressure.
- Intracranial hemorrhages: Bleeding within the brain, often caused by injuries or ruptured blood vessels, can increase ICP rapidly and significantly.
- Idiopathic Intracranial Hypertension (IIH): This condition, primarily affecting obese women of childbearing age, is characterized by increased ICP without an identifiable cause. It can lead to severe headaches and vision problems.
Symptoms and Diagnosis of Elevated ICP
The symptoms of increased intracranial pressure can vary widely depending on the underlying cause and the individual. Common symptoms include:
- Headaches: These are often severe and may be accompanied by nausea and vomiting.
- Vision problems: Individuals may experience blurred vision, double vision, or even temporary loss of vision.
- Confusion and disorientation: Elevated ICP can affect cognitive function, leading to confusion, memory issues, and difficulty concentrating.
- Seizures: In severe cases, increased ICP can trigger seizures.
- Papilledema: This refers to the swelling of the optic disc, which can be observed during an eye examination.
Diagnosing elevated ICP typically involves a combination of medical history evaluation, physical examination, and advanced imaging techniques such as CT scans or MRI scans. These imaging studies can provide detailed information about the brain's structure and any potential abnormalities.
Advanced Diagnostic Tools
In some cases, more specialized diagnostic tools may be employed. For instance, a lumbar puncture (also known as a spinal tap) can be used to measure CSF pressure directly. This procedure involves inserting a needle into the lower back to collect a sample of CSF, which can then be analyzed for various parameters, including pressure.
Additionally, intracranial pressure monitoring devices can be implanted temporarily to provide continuous ICP measurements. These devices are particularly useful in critical care settings, where real-time monitoring can guide treatment decisions.
Treatment and Management of Intracranial Pressure
The treatment approach for elevated intracranial pressure depends on the underlying cause. In many cases, a multidisciplinary team of healthcare professionals, including neurologists, neurosurgeons, and critical care specialists, is involved in managing these complex conditions.
Medications and Interventions
Medications play a crucial role in managing ICP. Osmotic diuretics, such as mannitol and glycerol, are often used to reduce ICP by drawing water out of the brain tissue and into the bloodstream, thus decreasing brain volume and pressure.
In cases of hydrocephalus, shunt systems may be implanted to divert excess CSF away from the brain, allowing it to be absorbed elsewhere in the body. These shunts can be life-saving for individuals with this condition.
For patients with traumatic brain injuries, immediate intervention is often necessary. This may include surgical procedures to remove hematomas (blood clots) or to relieve pressure by creating a temporary opening in the skull, known as a craniectomy.
Long-Term Management and Prevention
In addition to acute interventions, long-term management is crucial for many individuals with chronic conditions affecting ICP. This often involves regular follow-up appointments, ongoing medication regimens, and lifestyle modifications.
For instance, individuals with IIH may be advised to adopt a weight loss plan, as obesity is a significant risk factor for this condition. Additionally, managing comorbidities such as hypertension and diabetes is essential to overall health and ICP control.
Emerging Research and Future Directions

The field of intracranial pressure research is continually evolving, with new advancements offering hope for improved diagnosis and treatment.
Advanced Imaging Techniques
Recent developments in medical imaging have allowed for more precise and non-invasive assessment of ICP. For example, magnetic resonance elastography (MRE) is a technique that uses MRI to measure the mechanical properties of brain tissue, providing insights into ICP and brain health.
Additionally, diffusion tensor imaging (DTI) has been used to study the effects of ICP on white matter tracts, offering a more detailed understanding of the structural changes associated with elevated ICP.
Novel Treatment Approaches
Researchers are also exploring innovative treatment options. One such approach is the use of stem cell therapy to repair damaged brain tissue and reduce ICP. While still in its early stages, this therapy shows promise for individuals with traumatic brain injuries and other conditions causing elevated ICP.
Another area of interest is the development of biomarkers for ICP. Identifying specific molecules or genetic markers associated with ICP changes could lead to earlier and more accurate diagnosis, allowing for timely intervention.
Prevention and Public Health
Preventive measures are also a key focus in ICP research. This includes public health initiatives aimed at reducing traumatic brain injuries, such as promoting the use of helmets during sports and improving road safety.
Additionally, ongoing research is exploring the role of lifestyle factors, such as diet and exercise, in maintaining healthy ICP. For instance, studies suggest that a diet rich in antioxidants and omega-3 fatty acids may help reduce the risk of ICP-related conditions.
Conclusion
Understanding and managing cranial fluid pressure is a complex but crucial aspect of neuroscience and medicine. From the intricate mechanisms that regulate ICP to the various conditions that can disrupt this balance, this field offers a wealth of knowledge and ongoing research opportunities.
As our understanding of intracranial pressure continues to evolve, so too do our diagnostic and treatment capabilities. With ongoing research and advancements, we can hope for improved outcomes and a better quality of life for individuals affected by conditions impacting cranial fluid pressure.
What are the long-term effects of elevated intracranial pressure?
+Chronic elevation of intracranial pressure can lead to severe neurological complications, including cognitive impairments, vision loss, and even permanent brain damage. In severe cases, it can be life-threatening.
Can stress or anxiety affect intracranial pressure?
+While stress and anxiety themselves do not directly cause elevated ICP, they can exacerbate existing conditions or contribute to the development of symptoms. For example, stress may worsen headaches associated with increased ICP.
Are there any natural remedies for managing intracranial pressure?
+While there is no substitute for medical treatment, certain lifestyle modifications may help manage symptoms and reduce the risk of ICP-related conditions. This includes maintaining a healthy weight, managing stress, and adopting a brain-healthy diet rich in antioxidants and omega-3s.