Esophageal Leak
Esophageal leaks are a critical complication that can occur following esophageal surgery, particularly in patients undergoing esophagectomy or other reconstructive procedures. These leaks pose significant risks to patients' health and can lead to severe consequences if not promptly identified and managed. Understanding the causes, symptoms, and management strategies is crucial for healthcare professionals to provide optimal care and improve patient outcomes.
Understanding Esophageal Leaks

An esophageal leak refers to the breach or rupture in the esophageal wall, leading to the leakage of digestive contents, including gastric acid, enzymes, and food particles, into the surrounding tissues or the mediastinal space. This complication often arises postoperatively and can have a profound impact on the patient's recovery and overall health.
Esophageal leaks are a relatively rare but serious complication, with an incidence ranging from 5% to 20% depending on the surgical procedure and patient-specific factors. The severity of the leak can vary, from small, self-limiting defects to large, life-threatening ruptures. Prompt diagnosis and appropriate management are essential to prevent further complications and ensure the best possible prognosis.
Causes of Esophageal Leaks
The development of esophageal leaks is multifactorial and can be attributed to various surgical, anatomical, and patient-related factors. Common causes include:
- Surgical Technique: Inadequate surgical technique, such as improper suturing or anastomosis, can lead to leaks. Excessive tension on the esophageal tissue or insufficient blood supply to the anastomosis site may also contribute to leak formation.
- Anastomotic Necrosis: Necrosis or tissue death at the anastomotic site, often caused by ischemia or infection, can result in leakage. This is more common in patients with comorbidities like diabetes or those undergoing extensive surgical procedures.
- Anastomotic Stenosis: Narrowing of the anastomosis can restrict the passage of food, leading to increased pressure and potential leakage. This is often a result of scarring or inflammation at the surgical site.
- Infection: Bacterial or fungal infections can compromise the integrity of the esophageal wall, increasing the risk of leakage. Infections may be introduced during surgery or develop postoperatively.
- Patient Factors: Certain patient characteristics, such as advanced age, malnutrition, and immunosuppression, can increase the vulnerability of the esophageal tissue and contribute to leak formation.
Symptoms and Diagnosis
The symptoms of esophageal leaks can vary depending on the location and severity of the leak. Common clinical manifestations include:
- Fever: Patients often present with a high fever, indicating an inflammatory or infectious process.
- Chest Pain: Pain in the chest or upper abdomen, which may worsen with swallowing or deep breathing, is a frequent symptom.
- Dysphagia: Difficulty swallowing or a feeling of food getting stuck in the throat can indicate a potential leak.
- Increased Respiratory Symptoms: Patients may experience increased coughing, wheezing, or shortness of breath due to the leakage of gastric contents into the respiratory tract.
- Leakage: Visible leakage of gastric contents from the mouth or through a surgical drain can be a clear indicator of an esophageal leak.
Diagnosing esophageal leaks typically involves a combination of clinical assessment, imaging studies, and endoscopic evaluation. Common diagnostic tools include:
- Chest X-ray: Initial imaging may reveal signs of mediastinal widening or pleural effusion, suggesting a leak.
- Computed Tomography (CT) Scan: CT scans provide detailed images of the esophagus and surrounding structures, aiding in the identification of leaks and the assessment of their extent.
- Esophagram or Barium Swallow Study: This study involves the patient swallowing a contrast material (barium) to highlight the esophagus and detect any leaks or abnormalities.
- Endoscopy: Direct visualization of the esophageal mucosa and anastomosis site using an endoscope can confirm the presence and location of a leak.
Management and Treatment
The management of esophageal leaks is complex and requires a multidisciplinary approach involving surgeons, gastroenterologists, and critical care specialists. The primary goals of treatment are to control the leak, manage complications, and facilitate healing.
Initial management often involves conservative measures such as:
- Nutritional Support: Providing adequate nutrition is crucial to support healing. This may involve nasogastric or parenteral nutrition, depending on the patient's condition.
- Drainage: Surgical drains are often placed to collect and remove leaked fluids, reducing the risk of infection and promoting healing.
- Antibiotic Therapy: Broad-spectrum antibiotics are administered to prevent or treat infections associated with the leak.
- Fluid Management: Careful monitoring and management of fluid balance are essential to prevent dehydration and maintain optimal organ function.
In cases where conservative measures are insufficient, more invasive interventions may be required. These include:
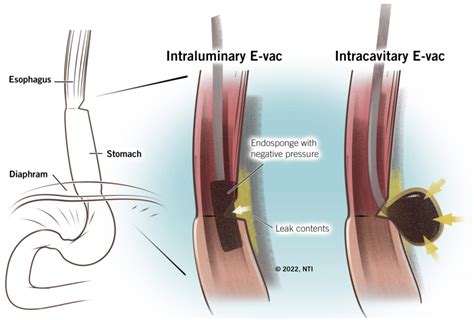
- Endoscopic Stenting: The placement of a stent across the anastomosis site can provide support and promote healing by reducing leakage.
- Surgical Revision: In severe cases, reoperation may be necessary to repair the leak, reinforce the anastomosis, or perform a bypass procedure.
- Vacuum-Assisted Closure (VAC) Therapy: This innovative technique involves the application of negative pressure to the leak site, promoting wound healing and reducing the risk of infection.
The choice of treatment approach depends on the patient's overall condition, the severity of the leak, and the resources available. Close monitoring and regular assessment are crucial to tailor the management plan to the individual patient's needs.
Prognosis and Long-Term Outcomes

The prognosis for patients with esophageal leaks depends on several factors, including the promptness of diagnosis, the severity of the leak, and the patient's underlying health status. With early detection and appropriate management, many patients can achieve successful healing and return to a good quality of life.
However, esophageal leaks can lead to significant complications, including mediastinitis (infection of the mediastinal space), pneumonia, respiratory distress, and sepsis. These complications can be life-threatening and require aggressive treatment. In some cases, despite optimal management, patients may experience persistent leaks or develop strictures, requiring ongoing care and interventions.
Long-term outcomes can be improved through comprehensive post-operative care, including close follow-up, nutritional support, and early intervention for any signs of leak recurrence or complications. Patient education and compliance with dietary and lifestyle modifications are also crucial for optimal healing and preventing future leaks.
| Statistic | Data |
|---|---|
| Incidence of Esophageal Leaks | 5% to 20% post-esophageal surgery |
| Risk Factors for Leaks | Advanced age, malnutrition, diabetes, extensive surgical procedures |
| Mortality Rate | 5% to 15% depending on leak severity and patient factors |

Frequently Asked Questions
What are the early signs of an esophageal leak?
+Early signs of an esophageal leak may include fever, chest pain, difficulty swallowing, and increased respiratory symptoms. Visible leakage of gastric contents can also indicate a potential leak.
How is an esophageal leak diagnosed?
+Diagnosis involves a combination of clinical assessment, imaging studies (such as CT scans and barium swallow studies), and endoscopic evaluation. These tools help identify the presence, location, and severity of the leak.
What are the treatment options for esophageal leaks?
+Treatment options include conservative measures like nutritional support and drainage, as well as more invasive interventions such as endoscopic stenting, surgical revision, and vacuum-assisted closure therapy. The choice of treatment depends on the patient’s condition and the severity of the leak.
What are the long-term outcomes for patients with esophageal leaks?
+Long-term outcomes vary depending on the severity of the leak and the patient’s overall health. With proper management, many patients can achieve successful healing and a good quality of life. However, persistent leaks or complications may require ongoing care and interventions.
How can patients prevent esophageal leaks post-surgery?
+While esophageal leaks can be challenging to prevent, patients can reduce their risk by maintaining good nutrition and overall health before surgery, following post-operative instructions carefully, and seeking prompt medical attention for any concerning symptoms.



