Posterior Lumbar Fusion With Instrumentation

Spinal fusion is a surgical procedure that has revolutionized the treatment of various spinal conditions, offering hope and improved quality of life for patients suffering from chronic back pain and spinal instability. Among the different techniques employed in spinal fusion, Posterior Lumbar Fusion with Instrumentation has emerged as a highly effective approach, providing stability and pain relief for individuals with lumbar spine issues.
This article delves into the intricacies of Posterior Lumbar Fusion with Instrumentation, exploring its definition, the conditions it addresses, the surgical process, and its remarkable outcomes. By examining real-world examples and industry insights, we aim to provide a comprehensive understanding of this innovative surgical technique, shedding light on its benefits and potential for revolutionizing spinal care.
Understanding Posterior Lumbar Fusion with Instrumentation

Posterior Lumbar Fusion with Instrumentation, often simply referred to as PLIF (Posterior Lumbar Interbody Fusion), is a sophisticated surgical technique designed to stabilize and reinforce the lumbar spine, the lower back region that bears much of the body’s weight and supports vital movements. This procedure is a cornerstone in spinal surgery, offering a durable solution for a range of spinal conditions.
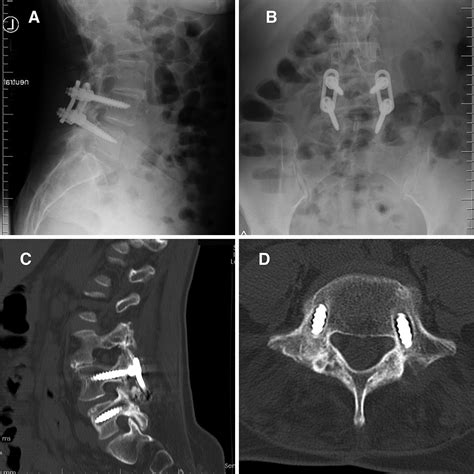
The term "Posterior" in PLIF indicates that the surgical approach is from the back of the patient, a common and effective method for accessing the lumbar spine. "Instrumentation" refers to the use of specialized devices, such as screws, rods, and plates, which are surgically implanted to provide immediate stability to the affected vertebrae. These instruments not only hold the vertebrae in the correct position but also facilitate the fusion process, allowing the bones to grow together and form a solid unit over time.
Conditions Addressed by PLIF
Posterior Lumbar Fusion with Instrumentation is a versatile surgical solution, effectively treating a variety of spinal conditions that cause pain and instability in the lumbar region. Some of the common indications for PLIF include:
- Degenerative Disc Disease: This is a natural process where the discs between the vertebrae lose their cushioning ability, leading to pain and instability. PLIF can effectively address this issue by replacing the degenerated disc with a bone graft or implant and stabilizing the spine with instrumentation.
- Spinal Stenosis: A condition characterized by the narrowing of the spinal canal, often causing compression of the spinal cord or nerve roots, leading to pain, numbness, and weakness. PLIF can alleviate these symptoms by creating more space in the spinal canal and stabilizing the affected vertebrae.
- Spondylolisthesis: A condition where one vertebra slips forward over the vertebra below it, causing instability and potential nerve compression. PLIF can correct this slippage and provide long-term stability.
- Traumatic Injuries: Severe spinal injuries, such as fractures or dislocations, can benefit from PLIF to stabilize the spine and prevent further damage.
- Infections or Tumors: In cases where spinal infections or tumors require surgical removal, PLIF can be employed to reconstruct the spine and ensure stability.
The Surgical Process

The surgical procedure for Posterior Lumbar Fusion with Instrumentation is a meticulously planned and executed operation, typically performed under general anesthesia. The patient is positioned face-down on a specialized surgical table, allowing the surgeon access to the lumbar spine from the back.
Step-by-Step Process
- Incision and Exposure: The surgeon makes a small incision in the midline of the lower back, carefully exposing the affected vertebrae. This incision is designed to be as minimally invasive as possible, minimizing trauma to the surrounding tissues.
- Decompression (if necessary): In cases where spinal stenosis or nerve compression is present, the surgeon may first perform a decompression procedure to relieve pressure on the spinal cord or nerve roots. This involves removing a portion of the lamina (the bony arch of the vertebra) and any other structures causing compression.
- Disc Preparation: The degenerated or damaged disc is carefully removed, and the space between the vertebrae is prepared for fusion. This involves clearing out any remaining disc material and ensuring a clean, stable environment for the fusion to occur.
- Implantation and Instrumentation: At this stage, the surgeon implants a bone graft or an interbody cage filled with bone graft material into the disc space. This graft acts as a scaffold, promoting the growth of new bone. Simultaneously, screws, rods, and plates are inserted to stabilize the vertebrae. These instruments provide immediate stability and guide the fusion process.
- Closure and Wound Care: Once the instrumentation and graft are in place, the surgeon carefully closes the incision, often using advanced techniques to minimize scarring and promote rapid healing. The patient is then transferred to the recovery area, where they are closely monitored.
Surgical Innovations
Over the years, Posterior Lumbar Fusion with Instrumentation has benefited from significant technological advancements, making the procedure even more precise and less invasive. These innovations include:
- Minimally Invasive Techniques: Surgeons now have the option to perform PLIF using minimally invasive surgical approaches, which involve smaller incisions and less tissue disruption. This leads to reduced pain, faster recovery times, and better cosmetic outcomes.
- Advanced Imaging and Navigation: Intraoperative imaging systems, such as fluoroscopy and computer-assisted navigation, allow surgeons to visualize the spine in real-time during the procedure. This enhances accuracy and safety, particularly when placing screws and other instrumentation.
- Biological Innovations: The use of advanced bone graft materials and growth factors has improved the success rate of fusion, reducing the risk of non-union and promoting faster healing.
Postoperative Care and Recovery
Posterior Lumbar Fusion with Instrumentation is a major surgical procedure, and patients can expect a dedicated postoperative care plan to support their recovery. This plan typically involves a combination of rest, medication, physical therapy, and lifestyle modifications.
Immediate Postoperative Care
Immediately after surgery, patients are closely monitored in the recovery room to ensure they wake up safely and comfortably. Pain management is a critical aspect of this phase, and patients are provided with medications to control pain effectively.
Patients may experience some discomfort and swelling at the incision site, which is normal. They are typically encouraged to start moving and walking within the first few days to prevent complications such as blood clots and to promote healing.
Physical Therapy and Rehabilitation
Physical therapy plays a crucial role in the recovery process. Patients are guided through a tailored exercise program designed to restore strength, flexibility, and stability to the lumbar spine. This program is progressive, starting with gentle range-of-motion exercises and gradually introducing more challenging activities as the patient heals.
The physical therapy team also educates patients on proper body mechanics and posture to prevent future strain on the lumbar spine.
Lifestyle Modifications
Following PLIF, patients are advised to make certain lifestyle adjustments to support their recovery and long-term spinal health. These may include:
- Avoiding high-impact activities and excessive bending or twisting for a specified period.
- Using proper lifting techniques to protect the spine.
- Maintaining a healthy weight to reduce stress on the lumbar spine.
- Engaging in low-impact exercises like swimming or walking to maintain fitness and spinal strength.
Outcomes and Benefits of Posterior Lumbar Fusion with Instrumentation
Posterior Lumbar Fusion with Instrumentation has consistently demonstrated excellent outcomes and a high level of patient satisfaction. This procedure offers a comprehensive solution for lumbar spine issues, providing:
- Pain Relief: One of the primary goals of PLIF is to alleviate chronic back pain. By stabilizing the spine and promoting fusion, this procedure can significantly reduce or eliminate pain, allowing patients to resume their daily activities with comfort and confidence.
- Stability and Function: The instrumentation used in PLIF provides immediate stability to the affected vertebrae, correcting deformities and preventing further slippage or instability. This enhanced stability can improve spinal function and overall quality of life.
- Improved Neurological Function: In cases of spinal stenosis or nerve compression, PLIF can effectively decompress the spinal canal, relieving pressure on the spinal cord or nerve roots. This can lead to improved neurological function, reducing symptoms like numbness, tingling, and weakness.
- High Fusion Rates: PLIF has consistently shown high fusion rates, with studies reporting successful bone fusion in over 90% of cases. This high success rate contributes to the long-term stability and durability of the procedure.
Real-World Success Stories
Real-world experiences of patients who have undergone Posterior Lumbar Fusion with Instrumentation paint a positive picture of the procedure’s effectiveness. Here are a few excerpts from patient testimonials:
"I had been living with chronic back pain for years, but after the PLIF procedure, I felt like a new person. The pain is gone, and I can finally enjoy activities I love without fear of aggravating my back."
"My life was transformed after the surgery. I went from being unable to walk without assistance to hiking and gardening again. The stability I gained from PLIF has given me back my independence."
Future Perspectives and Innovations
The field of spinal surgery, including Posterior Lumbar Fusion with Instrumentation, continues to evolve, driven by advancements in technology and a deeper understanding of spinal biomechanics. Here are some future perspectives and potential innovations in this field:
- Biological Agents: Ongoing research focuses on the development of advanced biological agents, such as stem cells and growth factors, to enhance the fusion process and reduce the risk of complications.
- Advanced Imaging and Planning: The integration of advanced imaging technologies, such as 3D printing and virtual reality, allows surgeons to plan and simulate surgeries with unparalleled precision. This can lead to even better outcomes and patient-specific treatments.
- Minimally Invasive Innovations: The trend towards minimally invasive techniques is expected to continue, with the development of new instruments and approaches that further reduce tissue disruption and accelerate recovery.
- Personalized Medicine: As our understanding of genetics and individual variations grows, spinal surgery may become increasingly personalized. Surgeons may be able to tailor procedures and implants to each patient's unique spinal anatomy and genetic profile.
In conclusion, Posterior Lumbar Fusion with Instrumentation is a testament to the remarkable advancements in spinal surgery. This procedure offers a durable solution for a range of lumbar spine conditions, providing pain relief, stability, and improved quality of life for patients. With ongoing research and technological advancements, the future of spinal care looks bright, promising even better outcomes and patient experiences.
How long does the recovery period typically last after Posterior Lumbar Fusion with Instrumentation?
+
The recovery period can vary depending on the individual and the extent of the surgery. On average, patients can expect to spend about 2-3 days in the hospital following the procedure. Full recovery, including returning to work and normal activities, can take anywhere from 6 weeks to 3 months. Physical therapy plays a crucial role in the recovery process, helping patients regain strength and mobility.
Are there any potential risks or complications associated with PLIF?
+
Like any surgical procedure, PLIF carries some risks. These may include infection, bleeding, nerve damage, or failure of the fusion to heal properly. However, these complications are relatively rare, and with advancements in surgical techniques and postoperative care, the success rate of PLIF has improved significantly.
How long does it take for the fusion to heal completely?
+
The fusion process can take several months to complete. While patients may feel significant pain relief and stability soon after the surgery, the bones continue to grow and fuse over time. Full fusion and stability are typically achieved within 6-12 months.
Can PLIF be performed on multiple levels of the spine at once?
+
Yes, PLIF can be performed on multiple levels of the spine in a single surgery. This is often necessary when multiple discs are degenerated or when there is instability across multiple vertebrae. The number of levels that can be fused in one surgery depends on various factors, including the patient’s overall health and the surgeon’s preference.
Are there any alternatives to PLIF for lumbar spine issues?
+
Yes, there are alternative surgical procedures for lumbar spine issues, such as anterior lumbar interbody fusion (ALIF) and transforaminal lumbar interbody fusion (TLIF). The choice of procedure depends on the specific condition, the patient’s anatomy, and the surgeon’s expertise. Each procedure has its own advantages and considerations, and a thorough evaluation is necessary to determine the most suitable approach for each patient.



