What Causes Poop To Leak Out
Unintentional leakage of fecal matter, commonly known as fecal incontinence, is a complex and sensitive issue that affects a significant number of individuals worldwide. It can be embarrassing and frustrating, impacting one's quality of life and self-esteem. Understanding the underlying causes of this condition is crucial for effective management and treatment.
Fecal incontinence refers to the inability to control bowel movements, resulting in involuntary leakage of stool. This condition can range from occasional minor leaks to complete loss of bowel control. It is more common than many realize, affecting people of all ages, but it is often underreported due to the stigma and shame associated with it.
Understanding Fecal Incontinence

The rectum and anus work together to store and control the passage of stool. When the rectum fills with stool, it stretches, triggering the urge to defecate. The internal and external anal sphincters then relax to allow the stool to pass through. In cases of fecal incontinence, this complex process is disrupted, leading to leakage.
Several factors can contribute to the development of fecal incontinence. These include damage to the muscles or nerves that control the anal sphincters, inflammation or injury to the rectum or anus, and issues with the functioning of the rectum itself.
Common Causes of Fecal Incontinence

Fecal incontinence can be caused by a variety of factors, some of which are more common than others. Here are some of the primary causes:
Damage to Anal Sphincters
The anal sphincters, composed of the internal and external sphincters, are crucial for maintaining bowel control. Damage to these muscles can result in weakness or loss of function, leading to fecal incontinence. Common causes of damage include:
- Childbirth: Vaginal childbirth can sometimes cause trauma to the anal sphincters, especially if forceps are used during delivery.
- Surgery: Surgical procedures near the anus, such as hemorrhoidectomy or fistula repair, can inadvertently damage the sphincters.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn's disease and ulcerative colitis can cause inflammation and scarring of the sphincters over time.
Nerve Damage
The nerves that control the anal sphincters can be affected by various conditions, leading to fecal incontinence. Some common causes include:
- Diabetes: This chronic condition can cause nerve damage, known as diabetic neuropathy, which may affect the nerves controlling the anal sphincters.
- Spinal Cord Injury: Damage to the spinal cord, whether due to trauma or disease, can disrupt the nerve signals responsible for bowel control.
- Multiple Sclerosis (MS): MS is an autoimmune disease that affects the central nervous system, potentially impacting the nerves involved in bowel control.
Rectal Prolapse
Rectal prolapse occurs when the rectum slips from its normal position and protrudes through the anus. This can interfere with the normal functioning of the anal sphincters and lead to fecal incontinence. Common causes include:
- Chronic Constipation: Straining during bowel movements can weaken the muscles and ligaments supporting the rectum, increasing the risk of prolapse.
- Aging: As we age, the muscles and tissues supporting the rectum can weaken, making prolapse more likely.
- Chronic Coughing or Sneezing: Persistent coughing or sneezing can put pressure on the rectum, increasing the risk of prolapse.
Diarrhea and Loose Stools
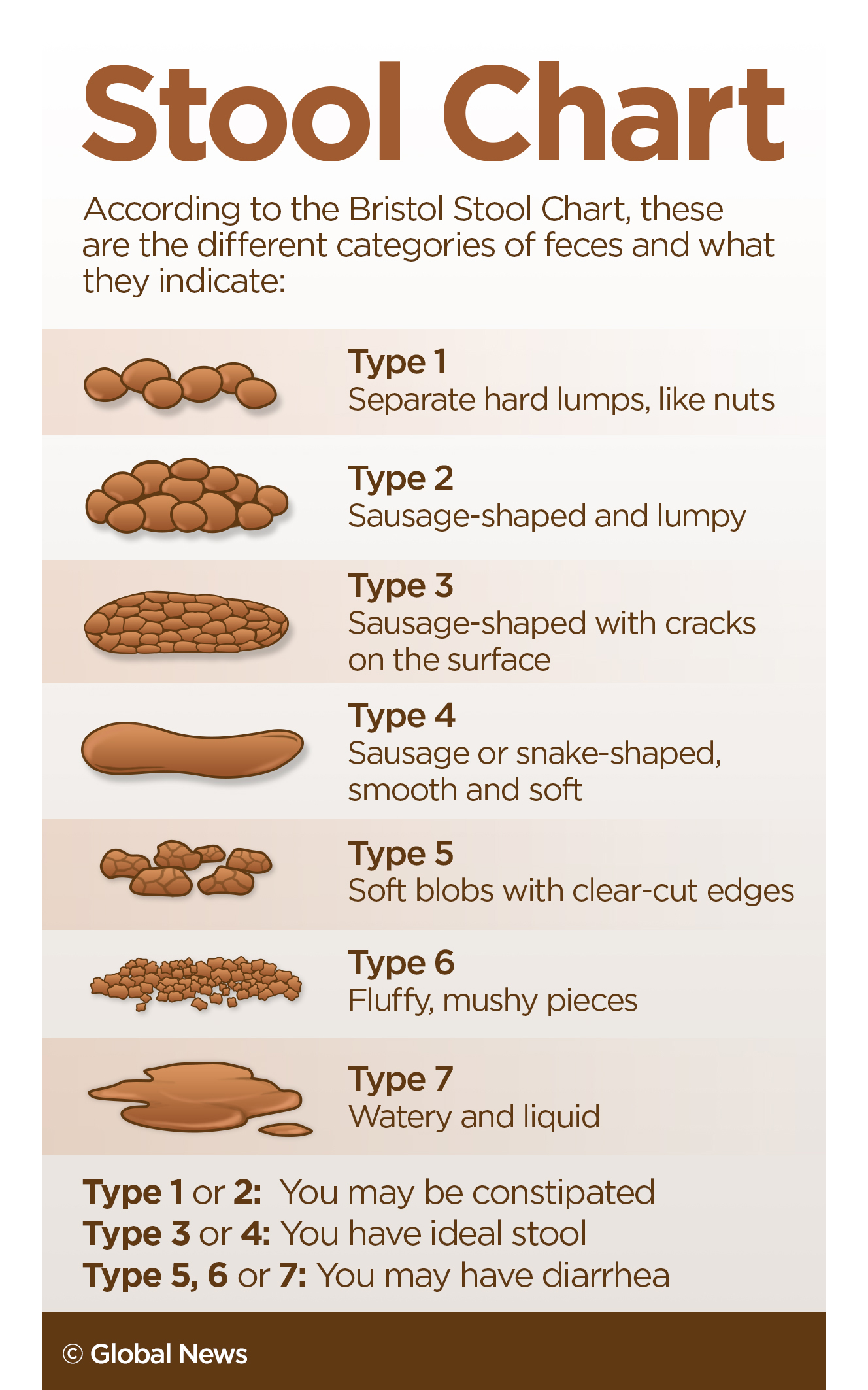
While diarrhea itself is not a cause of fecal incontinence, it can exacerbate the problem. Diarrhea can overwhelm the anal sphincters, making it difficult to control bowel movements. Common causes of diarrhea include:
- Infectious Diarrhea: Viral, bacterial, or parasitic infections can cause acute diarrhea.
- Food Intolerances: Conditions like lactose intolerance or celiac disease can lead to diarrhea when certain foods are consumed.
- Inflammatory Bowel Disease (IBD): Chronic inflammation in the digestive tract, as seen in conditions like Crohn's disease or ulcerative colitis, can cause diarrhea.
Other Factors
There are several other conditions and factors that can contribute to fecal incontinence, including:
- Constipation: Chronic constipation can lead to fecal impaction, where hardened stool blocks the rectum, making it difficult to pass softer stool.
- Radiation Therapy: Radiation to the pelvic area, often used to treat cancers like prostate or cervical cancer, can damage the rectum and sphincters.
- Certain Medications: Some medications, such as certain opioids or antidepressants, can cause constipation or diarrhea, which may contribute to fecal incontinence.
Diagnosis and Treatment
Diagnosing fecal incontinence typically involves a comprehensive evaluation by a healthcare professional. This may include a physical examination, medical history review, and various tests to assess the underlying cause. Common diagnostic tests include:
- Anal Manometry: This test measures the pressure and function of the anal sphincters.
- Colonoscopy: A procedure that allows the doctor to visually examine the inside of the colon and rectum.
- MRI or CT Scan: Imaging studies to assess the structure and function of the rectum and surrounding tissues.
Treatment for fecal incontinence depends on the underlying cause and the severity of the condition. It may involve a combination of lifestyle changes, medication, dietary adjustments, pelvic floor exercises, and, in some cases, surgical intervention. Here are some common treatment approaches:
- Dietary Modifications: Changing the diet to include more fiber and fluids can help regulate bowel movements and reduce diarrhea.
- Medication: Medications may be prescribed to manage underlying conditions like IBD or to control diarrhea or constipation.
- Pelvic Floor Therapy: Working with a physical therapist to strengthen the pelvic floor muscles can improve bowel control.
- Biofeedback: This technique uses sensors to provide real-time feedback on pelvic floor muscle activity, helping patients learn to control their muscles more effectively.
- Surgery: Surgical options may be considered for severe cases or when other treatments have not been effective. Surgical procedures can repair damaged sphincters or create a new sphincter mechanism.
Living with Fecal Incontinence
Fecal incontinence can have a significant impact on an individual's daily life and emotional well-being. It is important for those affected to know that they are not alone and that support is available. Here are some tips for managing fecal incontinence and improving quality of life:
- Seek Professional Help: Don't hesitate to consult a healthcare professional. They can provide guidance, support, and effective treatment options.
- Manage Diet: Work with a dietitian to develop a personalized diet plan that helps regulate bowel movements and reduces the risk of leakage.
- Practice Good Hygiene: Maintain proper hygiene to prevent skin irritation and infections. Use gentle, fragrance-free products specifically designed for sensitive skin.
- Use Protective Products: There are various incontinence products available, including pads, underwear, and liners, which can provide discreet protection and confidence.
- Join Support Groups: Connecting with others who are going through similar experiences can provide emotional support and practical advice.
Fecal incontinence is a complex condition with various potential causes. By understanding the underlying factors and seeking appropriate medical care, individuals can effectively manage their symptoms and improve their overall quality of life. Remember, there is no shame in seeking help, and with the right support and treatment, fecal incontinence can be successfully managed.
Can fecal incontinence be cured completely?
+In many cases, fecal incontinence can be effectively managed and improved, but a complete cure may not always be possible. Treatment approaches focus on managing symptoms and improving bowel control. With the right combination of therapies, many individuals can achieve significant relief and better quality of life.
Are there any home remedies for fecal incontinence?
+While home remedies may not cure fecal incontinence, they can help manage symptoms. These include maintaining a high-fiber diet, drinking plenty of fluids, and practicing regular pelvic floor exercises. However, it is important to consult a healthcare professional for proper diagnosis and treatment.
How can I prevent fecal incontinence?
+Preventing fecal incontinence involves maintaining good bowel health. This includes eating a balanced diet rich in fiber, staying hydrated, exercising regularly, and managing underlying conditions like diabetes or IBD. Additionally, avoiding excessive straining during bowel movements can help reduce the risk of damage to the anal sphincters.



