What Is A Pathological Fracture
Pathological fractures are a unique and often challenging aspect of orthopedic medicine. These fractures occur in bones that are weakened or affected by underlying medical conditions or diseases, making them susceptible to breakage even under normal or minimal stress. Unlike typical fractures resulting from acute trauma, pathological fractures are a result of the compromised integrity of the bone, often due to systemic illnesses or localized conditions affecting bone health.
Understanding pathological fractures is crucial for medical professionals, especially those specializing in orthopedics, as these fractures can present a range of diagnostic and treatment complexities. They are not only a marker of underlying disease but also a potential source of significant morbidity and, in some cases, mortality. Early recognition and appropriate management are key to improving patient outcomes and quality of life.
Understanding Pathological Fractures

Pathological fractures are a specific type of bone fracture that occurs in bones that have been weakened by disease or other underlying conditions. This makes them distinct from typical traumatic fractures, which result from an external force such as a fall or impact. The pathophysiology of these fractures is complex and often involves a combination of factors that contribute to bone fragility.
For instance, conditions like osteoporosis, which is characterized by a decrease in bone density, can significantly increase the risk of pathological fractures. This is because the bone becomes more porous and less able to withstand normal physiological loads, making even a minor fall or twist potentially fracture-causing. Similarly, certain cancers that metastasize to the bone can also lead to pathological fractures due to the cancer's destructive effect on the bone structure.
Causes and Risk Factors
Several medical conditions can lead to pathological fractures. These include:
- Osteoporosis: This is one of the most common causes, as it significantly reduces bone density and strength.
- Cancer: Cancers, particularly those that metastasize to the bone, can weaken it, making fractures more likely.
- Infections: Certain infections, such as osteomyelitis, can affect bone health and increase fracture risk.
- Metabolic Disorders: Conditions like renal osteodystrophy can alter bone metabolism, leading to fragility.
- Genetic Disorders: Some genetic conditions, like osteogenesis imperfecta, can cause brittle bones.
In addition to these conditions, certain medications, such as long-term corticosteroid use, can also increase the risk of pathological fractures by negatively affecting bone health. Advanced age is also a significant risk factor, as bone density naturally decreases with age, making older individuals more susceptible to these types of fractures.
| Condition | Impact on Bone Health |
|---|---|
| Osteoporosis | Decreased bone density, leading to fragile bones. |
| Cancer (Metastatic) | Destruction of bone structure, causing weakness. |
| Osteomyelitis | Bone infection that can compromise bone integrity. |
| Renal Osteodystrophy | Altered bone metabolism, resulting in weak bones. |
| Osteogenesis Imperfecta | Genetic disorder causing brittle bones. |

Clinical Presentation and Diagnosis
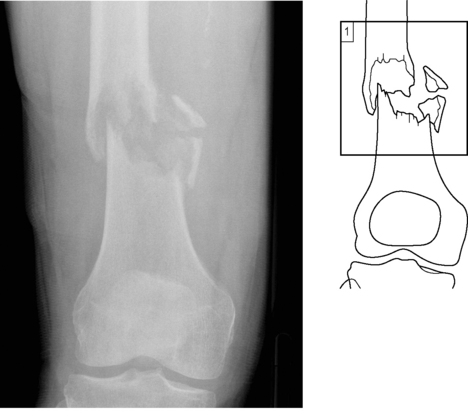
The clinical presentation of pathological fractures can vary widely depending on the underlying condition and the location of the fracture. Patients may present with sudden, severe pain in the affected area, especially if the fracture occurs during a minor trauma or even without any apparent cause. There might also be swelling, bruising, and a visible deformity at the fracture site.
Diagnosis typically involves a thorough medical history and physical examination. Imaging studies, such as X-rays, CT scans, or MRI, are crucial to confirming the fracture and evaluating the extent of bone damage. In cases where cancer is suspected, additional tests such as bone scans or biopsies may be necessary to determine the presence and extent of metastatic disease.
Treatment and Management

The treatment of pathological fractures involves a multidisciplinary approach, often requiring the collaboration of orthopedic surgeons, oncologists, endocrinologists, and other specialists. The primary goal is to stabilize the fracture, manage pain, and address the underlying condition to prevent further fractures.
Surgical Intervention
Surgery is often necessary to stabilize the fracture and prevent further displacement. The type of surgery depends on the location and severity of the fracture. For example, a hip fracture in an older adult with osteoporosis may require a hip replacement or internal fixation with screws and plates. In cases where cancer is the underlying cause, surgical options may be more limited, focusing on pain relief and maintaining function rather than complete fracture healing.
Medical Management
Medical management is a critical aspect of treating pathological fractures, especially when the underlying condition is a chronic disease. For instance, patients with osteoporosis may be prescribed medications like bisphosphonates or denosumab to improve bone density and reduce the risk of future fractures. Those with metastatic cancer may require chemotherapy, radiation therapy, or targeted therapies to control the disease and its effects on bone health.
Rehabilitation and Prevention
Rehabilitation plays a significant role in the management of pathological fractures. This includes physical therapy to restore mobility, strength, and function. Preventive measures are also crucial, especially for high-risk individuals. This can involve fall prevention strategies, such as home modifications, and the use of assistive devices. Additionally, maintaining a healthy lifestyle, including regular exercise and a balanced diet, can help improve bone health and reduce fracture risk.
Complications and Prognosis
Pathological fractures can lead to several complications, including infection, non-union (where the fracture fails to heal), and malunion (where the fracture heals in an incorrect position). These complications can further impair function and quality of life. The prognosis for pathological fractures depends on the underlying condition and the patient’s overall health. In cases where the underlying condition is well-controlled or in remission, the prognosis can be favorable. However, for progressive or advanced conditions, the prognosis may be guarded, with a higher risk of complications and a lower likelihood of complete recovery.
Future Implications and Research
Research in the field of pathological fractures is focused on improving diagnostic techniques, developing more effective treatments, and enhancing preventive measures. This includes the development of new medications to improve bone health, as well as advancements in imaging technology to better visualize and assess bone strength. Furthermore, ongoing research is investigating the role of genetic factors in bone fragility and the potential for personalized medicine approaches to treat pathological fractures.
In conclusion, pathological fractures are a complex and challenging aspect of orthopedic medicine. They require a comprehensive understanding of the underlying conditions, early recognition, and a multidisciplinary approach to treatment. With ongoing research and advancements in medical technology, the management of pathological fractures is evolving, offering improved outcomes and quality of life for affected individuals.
How are pathological fractures different from regular fractures?
+Pathological fractures occur in bones that are already weakened by disease or other conditions, making them more susceptible to breakage even under normal or minimal stress. Regular fractures, on the other hand, are typically caused by acute trauma or impact, such as a fall or accident, and do not necessarily involve pre-existing bone conditions.
What are the common signs and symptoms of a pathological fracture?
+Common signs and symptoms include sudden, severe pain in the affected area, swelling, bruising, and a visible deformity. The fracture may occur with minimal trauma or even without any apparent cause.
How are pathological fractures diagnosed and treated?
+Diagnosis involves a medical history, physical examination, and imaging studies like X-rays, CT scans, or MRI. Treatment is typically multidisciplinary, involving orthopedic surgeons, oncologists, and other specialists. It may include surgery to stabilize the fracture, medical management to address the underlying condition, and rehabilitation to restore function.



